Stories in Science Special Series
It takes a village: Creating engineered regulatory T cells to induce immune tolerance
Leonardo Ferreira: “What if we could avoid the need for HLA matching for successful organ transplantation without severely impairing the recipient’s immune system? Better even, what if we could use a mismatched HLA molecule present in the donor but not in the recipient and re-educate the recipient’s immune system to accept an organ with that foreign, non-self, HLA molecule as if it was part of the recipient, as if it was self?”

Leonardo M. R. Ferreira
Leonardo M. R. Ferreira, Ph.D. is an Assistant Professor of Microbiology and Immunology and, by courtesy, of Regenerative Medicine and Cell Biology at the Medical University of South Carolina and the Hollings Cancer Center. He holds a B.Sc. in biochemistry from University of Coimbra, Portugal, and a Ph.D. in biochemistry from Harvard University. His recent publication titled “Precision Engineering of an Anti-HLA-A2 Chimeric Antigen Receptor in Regulatory T Cells for Transplant Immune Tolerance” was published by Frontiers in Immunology on Sept 20, 2021. The narrative below explores the story behind the published work. You can follow him on Twitter @enhancerleo or visit his lab website.

Our immune system is usually seen as a highly organized army that protects us from foreign invaders, such as viruses and bacteria, as well as from cells deemed undesirable, such as stressed or cancerous cells or, more recently in history, cells transplanted from a different individual. This ability to distinguish self (our own tissues) from non-self (viruses, someone else’s cells) is at the core of the immune system. This is not always a black and white issue, however. Some elements are technically self, but are detrimental to the organism, such as stressed or cancerous cells, and are thus targeted for destruction – altered self.
Others are clearly not self, but they are invited guests, helpful to the organism, such as commensal bacteria, and tolerance to them is created – extended self. Disruptions to this delicate balance are involved in many diseases. It is as important to be able to mount an immune response against a pathogen as it is to not mount an immune response against our own healthy tissues. And it is as important to ramp up an immune response against an infectious agent as it is to dial it down once that agent has been eliminated. Yet, errors do happen. In autoimmune diseases, such as type 1 diabetes and multiple sclerosis, the patients’ own tissues are recognized and destroyed by their immune systems. In COVID-19 infections, sometimes the immune system is overzealous and causes profound tissue damage past elimination of SAR-CoV-2 virus.

Immune tolerance, a state of unresponsiveness to specific antigens (structures recognized by the immune system), is sometimes called the Holy Grail of immunology, precisely because of how hard it has been to accomplish. But the key to accomplish it might lie in a subset of T lymphocytes: regulatory T cells. These cells, also known as Tregs, are dedicated to suppressing specific immune responses. They do this using a panoply of mechanisms, from soaking up a molecule (cytokine) needed for T cell responses (interleukin-2) and secreting anti-inflammatory cytokines (interleukin-10, TGF-beta) to directly killing or otherwise disabling antigen-presenting cells required to activate T cells. This multi-factorial nature might be why it has been so difficult to induce true immune tolerance using conventional drugs. Could we then use Tregs as living drugs to achieve a cease-fire in autoimmune diseases?
Type 1 diabetes (T1D) is caused by the selective killing of the insulin-producing beta cells of the pancreas by auto-reactive T cells, leaving the patients dependent on daily insulin injections to control their blood glucose. Failure to do so can lead to nerve damage, amputation, blindness and, in extreme cases, death. There is no definitive cure for T1D. The intervention closest to a cure is a pancreas or an islet transplant (islets are only 2% of the pancreas and can be transplanted via the portal vein into the liver instead of the whole pancreas). However, this approach is not without problems, as these transplants face two types of immune rejection: allogeneic reaction, where the recipient’s immune system recognizes the islet graft as foreign, and autoimmunity, where the recipient’s immune system marks beta cells for destruction. Not addressing these immune dimensions in islet transplant would be the equivalent of building a sand castle by the ocean: no matter how well-built the castle is, the ocean waves will wash it away.
What if we could avoid the need for HLA matching for successful organ transplantation without severely impairing the recipient’s immune system?
Central to immune rejection are the major histocompatibility complex (MHC) molecules, also known as human leukocyte antigens (HLA) in humans. First crystallized and structurally characterized by one of my PhD advisors in the 1980s at Harvard University, Jack Strominger (together with Don Wiley and Pamela Bjorkman), HLA molecules can be thought of as billboard proteins on the surface of our cells presenting protein fragments, epitopes, to circulating T cells. This is how the immune system can tell self from non-self. HLA molecules themselves are highly polymorphic; there exist more than 3,000 HLA alleles, with each one of us carrying 18 of them. In organ transplantation, HLA must be matched between donor and recipient if acute rejection is to be avoided. In addition, the patients are put in a regimen where they take several immunosuppressive drugs every day for the rest of their lives, compromising their ability to fight infections and cancers. Chronic rejection, however, is far from being solved, as the immune system eventually figures out that those transplanted cells don’t look quite right (in addition to major, there are also minor histocompatibility antigens, which are much less understood, for example).
What if we could avoid the need for HLA matching for successful organ transplantation without severely impairing the recipient’s immune system? Better even, use a mismatched HLA molecule present in the donor but not in the recipient and re-educate the recipient’s immune system to accept an organ with that foreign, non-self, HLA molecule as if it was part of the recipient, as if it was self?
Given the complexity of the immune system, the perfect candidate to create this new state of immune tolerance would be a complex cell – the Treg. Work by my postdoctoral advisors in the early 2000s at the University of California San Francisco (UCSF), Qizhi Tang and Jeff Bluestone, showed that islet antigen-specific Tregs can prevent and even reverse (if coupled with pancreatic islet transplant) autoimmune diabetes in non-obese diabetic (NOD) mice. What would it take to translate this success to humans? As it turns out, there are a few hurdles. First, antigen-specific Tregs are exceedingly rare, especially in peripheral blood, the most commonly used medium to access immune cells. Second, Tregs divide much less ex vivo than conventional T cells do, and they can become unstable and lose their identity and suppressive function if cultured for too long. Third, in many cases the antigens recognized by Tregs that could be relevant for a given disease are not even known.
How can we bypass these hurdles? If obtaining enough antigen-specific Tregs is so hard and we don’t always know what antigen specificity is best anyway, can we direct Tregs to where we need them to go in a different way? The answer is yes. Great progress has been accomplished in the cancer therapy world by engineering killer T cells with a chimeric antigen receptor (CAR). A CAR is an artificial immune receptor consisting of an extracellular antigen-binding domain linked to an intracellular signaling domain, driving T cell activation upon target recognition. The most successful example of this man-made T cell specificity is the use of anti-CD19 CAR T cells to treat CD19-positive leukemia. In an analogous vein, one can use a CAR that recognizes a molecule on the surface of the tissue of interest to direct Tregs there and stimulate them to inhibit ongoing inflammation.
It was time for a more drastic approach.
In the labs of Qizhi Tang and Jeff Bluestone at UCSF, we chose to focus on HLA-A2 (which, by coincidence, was the first HLA molecule crystallized by Strominger, Wiley, and Bjorkman at Harvard) as the target for a CAR Treg. HLA-A2 is a common allele, found in 30% of the population. Transplanting islets from an HLA-A2-positive donor into an HLA-A2-negative T1D patient recipient would then allow for anti-HLA-A2 CAR Tregs, generated from the recipient’s peripheral blood, to specifically protect the transplanted islets from immune attack. For the antigen-binding domain of this anti-HLA-A2 CAR, we took the heavy chain and the light chain of the variable region of an anti-HLA-A2 antibody isolated from a sensitized individual, a pregnant woman. As it turns out, some women develop antibodies against HLA molecules uniquely present in the fetus they carry, that is HLA molecules derived from the father and not present in the mother. We fused these anti-HLA-A2 variable heavy and light chains with a linker peptide to create a “single-chain variable fragment” – scFv – the most common extracellular domain used in CARs, and molecularly cloned it in a CAR lentivirus vector backbone with a CD28-CD3 zeta signaling domain, the most common signaling domain used in CARs.
In an ideal world, we should be able to create anti-HLA-A2 CAR Tregs in no time. But not so fast with this CAR. After many months of tinkering with alternative peptide linkers and hinges together with Yannick Muller, a fellow postdoc in the Tang lab, this anti-HLA-A2 CAR just would not express on the surface of primary human T cells. It was time for a more drastic approach. Luckily for us, Jim Wells’ lab, which focuses on protein and antibody engineering, was just a short drive away from us at UCSF’s Mission Bay campus. Trastuzumab, also known as Herceptin, was the first monoclonal antibody against a cancer target, HER2, to be approved by the FDA. It has also served to derive an anti-HER2 scFv to construct an anti-HER2 CAR. The antigen-binding portion of an antibody is found in its variable region, which comprises a light and a heavy chain. If one zooms further in, each one of these variable regions contains three “complementarity-determining regions” – CDRs.
Those CDRs are what determines antibody specificity. Hence, in collaboration with the Wells lab, we replaced the CDRs of an anti-HER2 trastuzumab-based scFv with the CDRs of our anti-HLA-A2 antibody. To our relief, not only did this “grafted anti-HLA-A2 CAR” express well on the surface of primary human conventional T cells and Tregs, but it also had the same exact specificity as the parent anti-HLA-A2 scFv! Of note, we went to great lengths to assess this grafted anti-HLA-A2 CAR. There are thousands of HLA alleles and while they can all be distinguished by one’s immune system, there are also immunogenic surfaces, known as “eplets”, that are shared across several HLA alleles. In the business of allorecognition, it is important not just what the CAR recognizes, but also what it does not recognize. By using human cell lines and primary human islets with different HLA haplotypes, as well as beads individually decorated with different HLA alleles, we determined that our grafted anti-HLA-A2 CAR recognized HLA-A2 but not any other HLA molecule (with the exception of HLA-A28, which was also recognized by the original anti-HLA-A2 antibody via a shared eplet).
With these anti-HLA-A2 CAR Tregs finally in hand, it was time to finally put them to test: could they suppress immune responses in a specific manner? A common model to test human Treg suppressive function in vivo is xenogenic graft-vs-host disease (GvHD). Injecting human peripheral blood mononuclear cells (PBMCs) into an Immunodeficient mouse, the NOD scid gamma chain mutant (NSG) mouse strain, results in widespread tissue damage and eventually death of the animal, as human T cells recognize and destroy the foreign xenogeneic mouse tissues. Co-injection with human Tregs should prevent GvHD. We took this model with two refinements. On the Treg side, we did not introduce the grafted anti-HLA-A2 CAR into human Tregs using lentivirus, as is commonly done. Instead, we used CRISPR/Cas9 to make a double strand break in the endogenous TCR locus (using a protocol optimized in Alex Marson’s lab in our building at UCSF) and delivered the grafted anti-HLA-A2 CAR gene in the form of adeno-associated virus (AAV), a non-integrating virus, flanked by sequences matching those of the endogenous TCR locus – “homology-directed repair”.
In this fashion, instead of having a random number of copies integrating at random places in the genome with the lentiviral approach, we ensured that each CAR Treg had exactly one copy (during VDJ recombination in T cell development, one TCR alpha allele is silenced, a phenomenon known as “allelic exclusion”) of the CAR expressed under the same gene regulation rules as the endogenous TCR would. Moreover, this reprograms Treg specificity by removing the TCR and replacing it with the anti-HLA-A2 CAR, instead of just adding the CAR specificity on top of the pre-existing TCR specificity. On the mouse model side, we used HLA-A2-transgenic NSG mice (from Jackson Labs). This way, both the PBMCs from a third party donor and our reprogrammed anti-HLA-A2 CAR Tregs were activated by HLA-A2 present in the host tissue, a more stringent test of in vivo CAR Treg function than if the HLA-A2 had been present in the attacking PBMCs, the standard in the field. Co-injecting anti-HLA-A2 CAR Tregs with PBMCs with HLA-A2 present in the system reduced animal mortality in half by 3 weeks post-infusion, with almost half of the surviving animals living as long as 3 months. Highly effective! This showed that our anti-HLA-A2 CAR Tregs are immunosuppressive in vivo specifically when their target, HLA-A2, is present.
In spite of these encouraging findings, several obstacles remain to implementing engineered Treg-based therapy for T1D.
Now back to T1D. To date, there is no widely accepted robust model of T1D in humanized mice. Nevertheless, what we could do was to use a molecule, streptozotocin, that, once injected, kills off all the beta cells in NSG mice, rendering them diabetic. We then transplanted HLA-A2-positive human islets collected from cadaveric donors into the kidney capsule, a highly vascularized site, of these diabetic NSG mice. Luckily, human insulin works on mouse cells and hence the mice where the transplant was successful ceased to be diabetic. We then infused intravenously firefly luciferase-labeled anti-HLA-A2 CAR Tregs. Thanks to firefly luciferase, we could image the anti-HLA-A2 CAR Tregs non-invasively inside living animals using their bioluminescence! By a quirk of destiny, the COVID-19 lockdown in San Francisco started precisely as this experiment was ongoing. It mandated that only one person could be in the lab at a time. Through a system of shifts, online calendars, and many emails and video calls, we managed to tend to these mice every single day: they required human interleukin-2 (IL-2) injection twice a day (Tregs depend on IL-2 to survive and unfortunately mouse IL-2 does not work on human cells and the half-life of human IL-2 is only 15 minutes), blood glucose testing every other day, and bioluminescence imaging every other day. Nonetheless, the results were well worth it: as the weeks went by, we could see the anti-HLA-A2 CAR Tregs go first to the spleen (on the left side of the animals) and then home in the HLA-A2-expressing islet graft in the right kidney and remain there. No changes in blood glucose occurred, signifying that the anti-HLA-A2 CAR Tregs did not negatively impact the islets they interacted with.
In spite of these encouraging findings, several obstacles remain to implementing engineered Treg-based therapy for T1D. First, it will depend on the stage of the disease; if enough beta cell mass has already been lost, it will need to be accompanied by transplantation of pancreatic islets. Second, it has been often challenging to grow enough Tregs to hit a therapeutic dose. Third, T1D pancreatic islets are depleted in IL-2 and enriched in inflammatory cytokines, thus hostile to Treg survival and stability. Moreover, pancreatic islets are the site of insulin production and Tregs react poorly to insulin. Of note, it is not clear how abundant Tregs are in islets of either healthy or T1D patients, as they might act mostly at the level of the pancreatic draining lymph nodes. But that shouldn’t deter us from targeting Tregs to islets to curb inflammation there, as the goal is to treat T1D, not recapitulate physiology. Finally, if Tregs from T1D patients may be inherently defective, then are they really the best candidates to treat the disease? Should we be looking at ways to repair Tregs from T1D patients for autologous therapy, or generate universally compatible Tregs from healthy individuals for allogeneic therapy?
The prize is much too large not to carry on.
It took a village to create these engineered anti-HLA-A2 CAR Tregs for these proof-of-concept studies, and I know it will take an even larger one to translate these findings into patients. But this experience taught me that we scientists – despite all the competition and deep thinking inherent to science – can be formidable team players. By combining expertise, clearly communicating not only goals but also failures and short-comings, and coordinating tasks even in the face of a global pandemic and its restrictions to movement and face-to-face time, we were able to go from the white board into engineering anti-HLA-A2 CAR Tregs into existence. The prize is much too large not to carry on. If successful, it could be the first in a wave of approaches using cells as living drugs to truly re-educate the immune systems of patients suffering from autoimmunity and inflammation.
The CS Media Lab is a Boston-anchored civic science news collective with local, national and global coverage on TV, digital print, and radio through CivicSciTV, CivicSciTimes, and CivicSciRadio. Programs include Questions of the Day, Changemakers, QuickTake, Consider This Next, Stories in Science, Sai Resident Collective and more.

-
 Audio Studio1 month ago
Audio Studio1 month ago“Reading it opened up a whole new world.” Kim Steele on building her company ‘Documentaries Don’t Work’
-
Civic Science Observer1 week ago
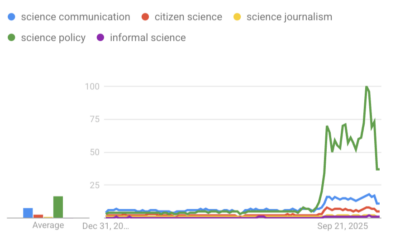
‘Science policy’ Google searches spiked in 2025. What does that mean?
-
Civic Science Observer1 month ago
Our developing civic science photojournalism experiment: Photos from 2025
-
Civic Science Observer1 month ago
Together again: Day 1 of the 2025 ASTC conference in black and white
Contact
Menu
Designed with WordPress